Why Does My Tooth Hurt When I Drink Cold Water?
Last Updated: January 5, 2026
🕒 7 min read

🚀 Short answer
Cold water doesn’t cause disease — it causes reactions.
Even healthy teeth can react to cold, and that can be completely normal.
The trick is knowing whether your tooth is just sensitive… or asking for help.
Most of the time, it’s nothing serious. Just a cold water hitting a sensitive spot on your tooth.
But sometimes, it signals a problem that needs attention.
⚡ Short-lasting pain (under 5 seconds)
If the pain is sharp, intense, and stops almost immediately after the cold is gone, this is your first big clue.
On a pain scale from 1–10, this usually sits between 4 and 8, but it disappears fast.
That timing matters more than the intensity.
If the pain lingers and stays longer than 5 seconds, skip this section and jump to long-lasting pain below.
The most common cause: the neck of the tooth

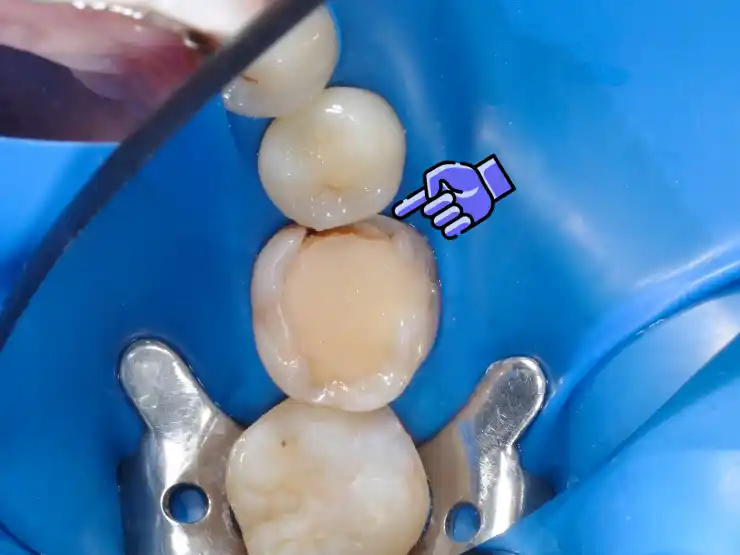
Blue area roughly represents the neck of the tooth. The neck of the tooth is the most common source of cold sensitivity.
Most short, cold-triggered pain comes from the neck of the tooth —
the area where the tooth meets the gums.
Sometimes nothing is “wrong.”
Very cold water hitting a very sensitive spot can hurt, even on a healthy tooth.
Usually this is mild nad it doesn’t happen every time you drink cold water.
Receding gums
Second most common cause is gum recession.
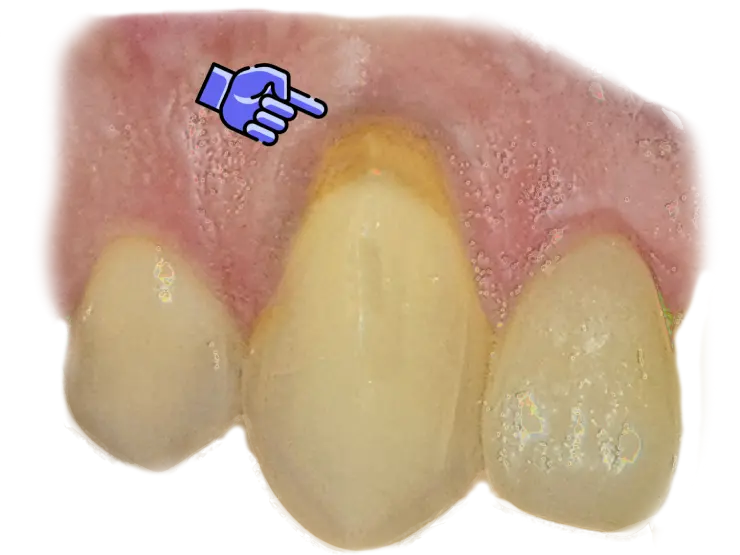
Points to receding gums, where gum line has pulled back exposing the neck of the tooth.
When gums pull back, they expose a part of the tooth that was never meant to be exposed.
That surface reacts fast — and loudly — to cold.
But after the cold is gone, the pain usually stops quickly.
This is extremely common and most of the time not an emergency, so no need to worry over it.
After some time, this place on the tooth gets mineralized and sensitivity reduces.
So it doesn’t mean that if you have receding gums, you will have permanent sensitivity.
Receding gums - How to check this yourself
If you’re a DIY type (like myself) and you want to confirm it yourself:
- Stand in front of a mirror.
- Gently pull your lip or cheek away from the area where you felt pain.
- Look for a tooth that appears:
- Longer/Taller than the others
- Or longer/taller than the same tooth on the opposite side
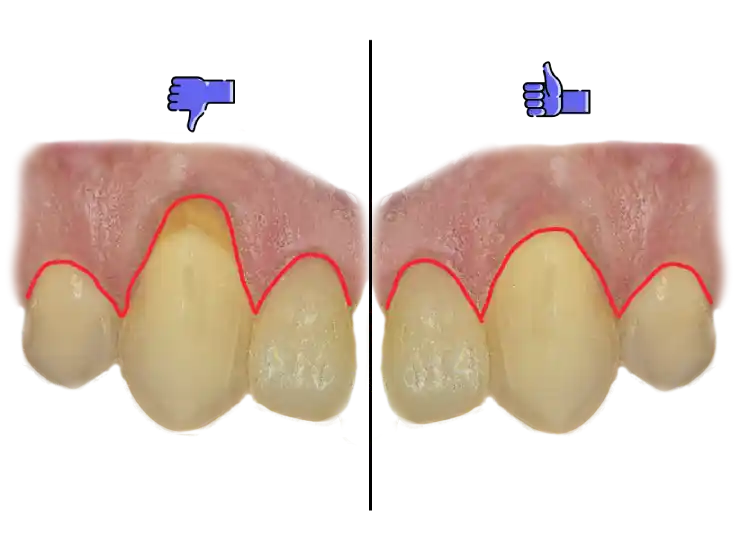
You can see the gum line is higher on the left side tooth compared to the right side tooth and the color of the tooth material in that area is different.
If gums have receded, you may notice:
- The gum line sitting higher if upper jaw, or lower if lower jaw, than usual
- A different color or texture near the gum line
(this area isn’t enamel — it’s more sensitive material underneath)
This doesn’t replace a dental exam.
It just helps you understand what’s likely going on and what can you do next.
Receding gums cause
Most common cause of receding gums is brushing too hard.
Using a hard-bristled toothbrush or brushing with too much force wears away gum tissue.
So make sure to use a soft-bristled toothbrush and brush gently. Other causes include:
- Tooth position causing excessive force on gums
- Gum disease (gingivitis or periodontitis) can cause gum recession
- Hormonal changes (pregnancy, menopause)
- Poor oral hygiene leading to plaque buildup and tartar formation that are pushing gums away from teeth
🦷 Found receding gums — what now?
First, the uncomfortable truth:
Gums don’t grow back on their own.
In most cases, the goal isn’t reversal — it’s stopping progression and reducing sensitivity.
Yes, gum graft surgery exists.
And yes, it can restore the gum line.
But:
- It’s not guaranteed long-term
- Results can relapse
- It’s usually reserved for significant functional or esthetic problems
If your main goal is simply drinking cold water without pain, surgery is rarely the first or best option.
Practical ways to reduce sensitivity
1. Desensitizer (fastest option) 🚀
This is the quickest, simplest, and most effective solution.
A dentist applies a thin layer of desensitizing material to the exposed area, wait a few minutes to work its magic and it’s done.
It seals microscopic channels in the tooth surface, isolating nerve endings.
- Painless
- Takes minutes
- Relief is often immediate
Most dental offices have this.
2. Toothpaste for sensitive or receding gums
If you prefer to avoid the dentist anytime possible (as most do) — and the pain is tolerable — this is a valid option.
You can easily get this toothpaste at any drugstore, usually labeled for sensitive teeth.

- Use a soft toothbrush
- Brush gently, focusing on the sensitive area
- Be patient
It usually takes 2–4 weeks to notice improvement.
Sometimes longer.
Slow, but effective for many people.
3. Dentist again - Filling or restorative coverage
If sensitivity returns quickly or becomes disruptive, a dentist may place a small layer of filling material over the exposed area.
- Local anesthesia is used
- Relief is immediate
- This creates a physical barrier over the sensitive surface
This option is typically used when simpler measures don’t last.
❄️ Other cases of cold sensitivity
As mentioned, most of the times it’s about really cold water hitting very sensitive spot on the neck of a tooth.
Second most common cause is receding gums, which then expose sensitive tooth surfaces.
But sometimes, there are other causes that triggers cold sensitivity.
Pay attention if:
- Pain is very strong (8–10/10)
- Pain lingers after the cold is gone
Possible causes include:
White spots on teeth
These areas have altered structure and can be highly sensitive.

Possible cause of cold sensitivity: white spot on tooth surface.
Tooth decay (cavities)
Early decay causes mild, short sensitivity.
Deeper decay can cause stronger pain.
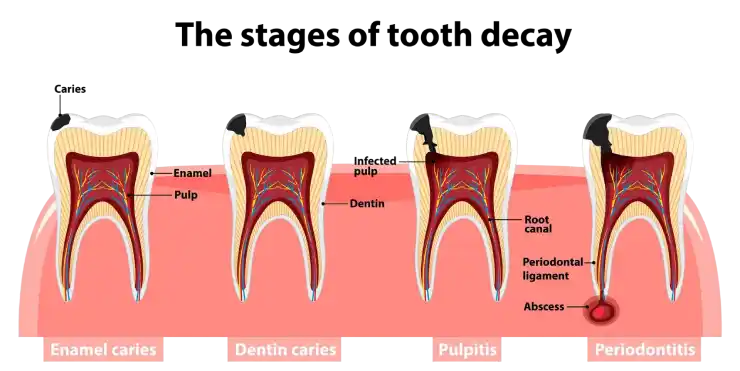
1.Enamel decay can be even without symptoms - that's why regular dentist checkups are important. 2.Dentin decay is often sensitive to cold and it can be more sensitive as it gets deeper to the nerve - right time to pick up the phone and call the dentist. 3. Tooth nerve inflammation - severe pain, painkillers needed, best pain relief is to see the dentist and prevent the root infection. 4. Abscess formation - swelling, severe pain, emergency dental treatment needed.
Usually it’s hard to find it yourself since it can be just some discoloration present, or it is located between the teeth which is hard even for the dentist to spot without a x-ray.
If you see a hole or dark spot — don’t wait!
The only solution here is to see a dentist to remove decay and put the filling asap so it doesn’t progress to the tooth nerve causing more pain and more expensive root canal treatment.
Tooth cracks
Cracks aren’t always visible.
It could be just a line on the tooth surface which is hard to see, only when a strong light is shined at the right angle.

Typical signs:
- Sharp pain on cold, but also on hot, sweet, or sour foods/drinks
- Additionally to other causes, here is sensitivity when chewing
- Pain that comes suddenly and disappears quickly
Cracks tend to get worse over time. Early treatment matters.
Cracked or failing fillings
When a filling cracks or loses its seal, cold reaches sensitive areas.
A cracked filling exposes sensitive tooth areas, causing cold pain.That pain is a warning — fix it now, before decay turns a small problem into a big one.
Worse than that, food gets trapped in the gap where the filling fell off.
In such cases, decay accelerates fast since you can’t clean the area with a tooth brush.
This requires dental repair — delaying usually makes it worse.
Professional teeth cleaning
After calculus removal, teeth may feel sensitive on cold for a few days.

Professional teeth cleaning procedure removes the hardened plaque (calculus) and other deposits that can't be removed with regular brushing. So this procedure is important for your teeth and gums health, and potential sensitivity after the procedure is a worthy tradeoff.
This is normal.
Once natural remineralization starts, sensitivity usually fades.
Sensitive-teeth toothpaste can help during this phase.
Teeth whitening
Temporary sensitivity is common after whitening.
Usually resolves in 2–7 days.

Teeth whitening is a chemical process that on microscopic level dries out the tooth structure which causes temporary sensitivity to cold.
Do note:
- If the sensitivity is high (you need a painkiller to bear it),
- or it is getting worse and worse over time
- or it lasts for more than a week
schedule a dentist appointment.
It can be that one of your teeth overreacted to the procedure and it needs to be treated.
⏳ Long-lasting pain (over 5 seconds)
This category deserves attention.

1. Advanced tooth decay
If pain lingers 10/15/20–60 seconds after cold, decay is likely deep.
This is your window to:
- Treat the decay
- Possibly avoid root canal treatment
- Often it needs a root canal treatment, but you can avoid having an abscess or infection develop
Delaying reduces options.
2. Tooth nerve inflammation
The pain is severe, it can stay for some time, the tooth can start hurting even on it’s own, you can’t sleep, not to mention cold water…
Just seek for the dentist, please don’t hesitate, it can help you a lot and the procedure is straight forward and you will get your pain relief.
✅ Bottom line
Cold sensitivity isn’t mysterious.
Your tooth is reacting to exposure, damage, or inflammation.
The most important clue isn’t how strong the pain is — it’s how long it lasts:
- Pain that stops quickly is often manageable
- Pain that sticks around after the cold is gone needs a dental check
Ignore intensity.
Watch the timing.
And when in doubt — get a diagnosis before guessing turns into regret.
Author: DMD Alexander K.
Doctor of Dental Medicine on dental topics. Facts first. Drama optional.
Learn more on the About page.